Strengthening psychiatric care with patient input and team-based approach
The clinical team from Mount Sinai's Inpatient Psychiatry Unit
Inpatient Psychiatry Unit receives top ranking in quality of care and services provided
Distressed. Overwhelmed. Frightened. That’s how Adrienne Shulman felt when she was first admitted to Mount Sinai’s inpatient psychiatry unit over 20 years ago. Today, healthy and active, she supports that same unit by helping to address those feelings as Mount Sinai’s first psychiatric Patient Support Specialist.
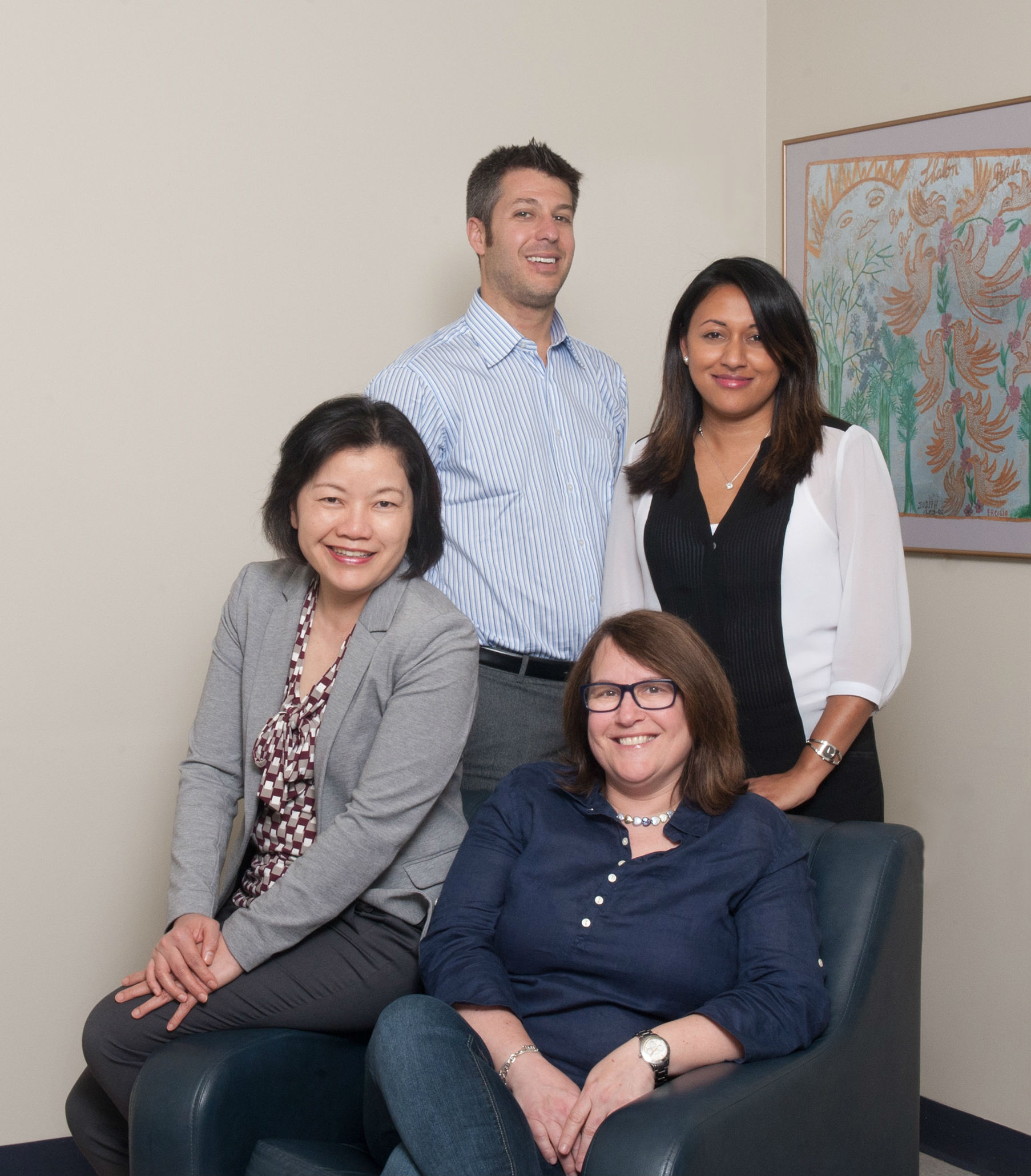
Her efforts are an added resource to the robust team-based approach of the unit’s clinicians, led by Dr. Greg Chandler, Director of Inpatient Psychiatry, with Ping Rau, the Nursing Unit Administrator; and Natasha Persaud, Clinical Nurse Specialist. The team has improved the patient experience by being responsive to patient needs and feedback. These efforts were recently highlighted by a National Research Corporation Canada’s (NRCC) report, which measures performance based on patient perceptions across Ontario: the unit received the top ranking in quality of care and services provided.
“As a team, we are very gratified by our top ranking by patients. It means that our work to ensure a patient-centred approach is having real impact,” said Dr. Chandler. “This is part of our effort to offer our patients a full spectrum treatment, addressing their psychological, medical and social needs with a unified approach.”
Clockwise: Dr. Greg Chandler, Natasha Persaud, Adrienne Shulman and Ping Rau
Patient support
As a former patient of the unit herself, Ms. Shulman knows exactly what patients are going through and works with patients to help make the process of admission, treatment and discharge less “overwhelming and scary”.
“This has been an incredible opportunity to pay it forward by taking my lived experience and using it to help demystify what it’s like to be a patient," she noted. “Mount Sinai helped me more than I can say. I never thought I could have a fulfilling life, but the treatment I received here has helped me do just that. This is the best way I know how to give back to the unit that took such exemplary care of both me and my family.”
By meeting with patients and working with the psychiatry unit’s clinicians, Ms. Shulman helps patients better understand their journey. She also supports family members of patients in the unit, facilitating the important role that they can play in treatment and recovery. She has also helped establish a patient feedback group to deal with important issues immediately.
For example, when patients and family members revealed that they felt overwhelmed and confused by the number of staff members working on the unit, Ms. Shulman and the Patient and Family-Centred Committee suggested photos and brief bios of all the staff.
Better together
These staff members are the foundation of the unit’s success. Both Dr. Chandler and Ms. Rau emphasize that the improvements have been a result of a highly collaborative team approach.
“When we see patients, it’s often as a full clinical team,” explained Dr. Chandler. “It helps us offer more consistent and tailored treatment because we’re all in the room together, hearing the same things from our patients and working together to address their needs. It’s having a very positive impact on the quality of care.”
Efforts like these have increased teamwork with other units in the hospital, including emergency, medicine, geriatrics, and outpatient psychiatry.
In addition to improving collaboration and communications between staff and with patients, the unit staff looked at how they can streamline processes to increase efficiency.
Planning ahead
Natasha Persaud, Clinical Nurse Specialist, highlights the example of discharge planning. “We have implemented various strategies, such as daily team rounds and patient whiteboards, to facilitate proactive discharge planning right from the time of admission,” she said. “We are constantly working to make more resources available to our patients, so we can better support them when they leave the unit and transition back to the community.”
Ongoing improvements
“This is all part of our ongoing quality improvement efforts,” said Ms. Rau. “We’re constantly looking for ways to better serve our patients.”
“Collaboration and proactive planning help us treat patients more efficiently, which means they spend less time in the unit and we can treat more patients,” added Dr. Chandler.
These are just a few of the many initiatives that helped Mount Sinai’s Psychiatry Department continually improve its patient satisfaction ratings and outcomes. The NRCC recognized this in its report, which is designed to highlight Ontario hospitals with excellent performance ratings, based on patient perceptions, so that others can identify and learn from these leading practices.